Despite the fact that modern medicine has created a number of powerful and effective drugs for the treatment of pancreatitis, without diet, such treatment is less effective. Moreover, with a mild or moderate course of pancreatitis, treatment may even consist of one nutritional correction.
Unfortunately, many patients follow the diet only while in the hospital, while after discharge they stop it and, referring to their recovery, consume prohibited foods. As a result, this leads to repeated inflammation, which is much more difficult to treat than the primary one.
The importance of proper nutrition in pancreatitis
Acute and chronic pancreatitis is treated mainly with medications, and in some cases, surgical assistance is required. However, neither drug therapy nor surgical treatment is absolutely ineffective without correction of the patient's diet.
A diet is prescribed, without exception, to every patient with pancreatitis, regardless of the severity of the disease. Non-compliance leads to a second attack of the disease, which the patient will tolerate much worse than the initial one.

The diet allows you to reduce the load not only on the pancreas, but also on the entire gastrointestinal tract system as a whole. In addition, the selection of foods in the diet is aimed at providing the patient's body with all the necessary substances for the regeneration of damaged organs.
In many patients, the disease in the acute period causes such serious damage to the pancreas that the patient's diet is prescribed for life. Patients who ignore the doctor's prescriptions regarding the diet in such a situation may remain disabled, or even die.
A simple conclusion follows from this: a diet for pancreatitis (both acute and chronic) is not just recommended, but necessary.
Who Prescribes the Diet?
Only a doctor can prescribe a diet and certain recipes for pancreatitis. At the same time, in this case, doctors of several specializations are suitable: therapists, endocrinologists, gastroenterologists and, in some cases, infectious disease specialists.
Self-prescribing a diet is dangerous both for health (disability is possible) and for life. It is especially dangerous to prescribe a diet for pancreatitis without consulting a doctor for children and pregnant women.
Features of the diet for acute pancreatitis
A distinctive feature of the diet for acute pancreatitis can be called a reference point towards fasting. That is, in acute pancreatitis, the diet should contain the most gentle food for the gastrointestinal tract in general and the pancreas in particular.
Moreover, doctors prescribe to minimize the amount of food consumed in the first week of illness, and in the first 2-4 days of illness, complete starvation can be prescribed at all (you can only drink).

The goal of this fairly restrictive diet is simple - to significantly reduce the stress on the pancreas. In the absence of a diet in the acute phase of pancreatitis, treatment may be completely useless.
Features of the diet for chronic pancreatitis
The peculiarities of nutrition in chronic pancreatitis are that the patient needs to limit himself in the use of fatty, fried, spicy and smoked foods throughout his life.
In this case, the patient is allowed to sometimes eat such food, but in small quantities. Alcohol is completely contraindicated, but most patients ignore this prescription, so doctors simply insist that the patient drink it as little as possible and in small quantities.
Features of the diet with exacerbation of pancreatitis
With an exacerbation of pancreatitis, an extremely restrictive diet is introduced, in which in the first days of the disease it is recommended to completely refuse to eat. Further, during the week, it is allowed to use only low-fat broths, cereals (usually buckwheat) and mashed potatoes.
After the exacerbation subsides, the patient should smoothly switch to a standard diet for chronic pancreatitis. Moreover, all changes in nutrition during an exacerbation of pancreatitis should be carried out exclusively in consultation with a doctor. Self-administration of diet therapy is dangerous not only for health, but also for life.
What can not be done with pancreatitis?
With pancreatitis of any type, there is a fairly large list of products that are strictly prohibited to use (both until the end of treatment, and, much less often, for life).
The list of foods prohibited for pancreatitis is as follows:
- Fatty meats, fried meat (cutlets also fall here), canned food, sausages, smoked products, stew.
- Fatty fish, smoked and salted fish, any canned fish and caviar.
- Fatty varieties of cottage cheese, curds (glazed curds are especially dangerous), spicy and smoked types of cheese.
- Scrambled eggs or hard-boiled eggs.
- Turnip, garlic, onion, horseradish, pepper, radish.
- Beans, beans, mushrooms.
- Raw and not frayed fruits, sour and overly sweet fruits (oranges, figs, grapes, for example).
- Rolls, cakes, as well as other sweet and / or fatty (due to cream) confectionery products.
- Chocolate, ice cream, nuts.
What can and is useful to eat with pancreatitis?
With pancreatitis, the following foods are allowed:
- soups from cereals and vegetables;
- boiled meat from beef, fish, poultry;
- chicken egg omelet;
- a small amount of honey;
- various cereals;
- baked or boiled vegetables;
- mashed potatoes;
- carrot.
What can and cannot be drunk?
The use of the following drinks is prohibited:
- any alcoholic drinks;
- sweet and carbonated drinks (including shop juices);
- cocoa;
- coffee drinks.
The following drinks are allowed:
- kefir;
- weak black and green tea;
- rosehip decoctions;
- compote;
- curdled milk.
Alcohol
Alcohol with pancreatitis is contraindicated in any form of the disease. Alcoholic beverages have a detrimental effect not only on the pancreas, but also on the adjacent organs of the abdominal cavity, which in the vast majority of cases are also indirectly affected by pancreatitis.

Alcohol consumption against the background of chronic pancreatitis increases the severity of its symptoms and leads to the progression of the disease. Alcohol consumption in acute pancreatitis significantly reduces the effectiveness of treatment and increases the risk of death from pancreatic necrosis.
Sweet and honey
Honey and sweets (excluding chocolate) are allowed to be consumed only with chronic pancreatitis. In the acute form of the disease or exacerbation of chronic pancreatitis, any sweets, including honey, should be excluded.
In addition, with chronic pancreatitis, sweets can be eaten only in limited quantities, as rarely as possible. The fact is that if the pancreas is damaged against the background of chronic pancreatitis, the use of sweets is a dangerously high risk of diabetes mellitus.
Dairy products
Although whole milk can be consumed, it is not recommended, since it often provokes diarrhea and flatulence. It is recommended to consume low-fat kefir, fermented baked milk and yogurt, no more than one glass a day.
Also, from dairy products with pancreatitis, cottage cheese (up to 9% fat) and cheese (mild varieties, such as mozzarella, Adyghe and feta cheese) are allowed. Sour cream can be consumed only one spoonful a day, but only as an additive for soups.
Porridge
With this disease, only some types of cereals are allowed (buckwheat, semolina, rice and oatmeal). Moreover, porridge can only be cooked in water or milk, in a 1 to 1 ratio.

In the chronic form of the disease, corn or barley porridge can be consumed once a week. But pearl barley and millet porridge is prohibited for any form of pancreatitis.
Oils
With pancreatitis, it is allowed to add a small amount of butter to the dishes. Vegetable and olive oil can also be added in small quantities to dishes, but only for the chronic form of the disease.
Sea buckthorn oil is strictly prohibited for pancreatitis due to stomach irritation and creating a serious load on the pancreas.
Baking, biscuits
Even with acute pancreatitis, after several days of hunger strike, certain types of pastries and cookies are allowed. Namely:
- white or slightly dried bread;
- uncooked and unsweetened cookies;
- biscuit biscuits.
Other baked goods and baked goods are either prohibited or simply not recommended. Fresh baked goods are especially dangerous, which can significantly aggravate acute pancreatitis or provoke an exacerbation of chronic pancreatitis.
Vegetables
It is allowed to eat vegetables only in boiled or baked form, but it is much better to use them in pureed form (mashed potatoes, casseroles, soups).

The following vegetables are allowed for consumption:
- potato;
- carrot;
- beet;
- pumpkin;
- cauliflower;
- green pea;
- zucchini.
In a limited amount and only in case of chronic pancreatitis, outside exacerbations, it is allowed to use white cabbage and tomatoes, but only in boiled form.
Fruits
With pancreatitis, it is allowed to eat fruits baked or in the form of compotes and jelly. Fruit puree is also allowed. In limited quantities, you can eat a melon or watermelon.
Sour fruits (citrus fruits) are completely contraindicated, including juices made from them. It is also important to consider that it is prohibited to use raw fruits for acute pancreatitis or exacerbation of chronic pancreatitis.
Dried fruits
In acute pancreatitis, dried fruits are strictly prohibited, while in the chronic form of this disease, they can be consumed only in the form of compotes.
The fact is that dried fruits contain not much less fiber than fresh fruits. Fiber is contraindicated in pancreatitis.

It is also worth considering that, although in the chronic form of the disease, dried fruits are allowed in small quantities, there are those dried fruits that cannot be consumed at all (figs, dates, raisins, dried apricots).
Nuts
Nuts are a rather fatty product, which immediately speaks against their use for pancreatitis. They can be consumed only in the chronic form of the disease and only in small quantities. But here, too, there are some nuances.
So doctors prohibit the use of nuts for a year after acute pancreatitis or for a year after suffering an exacerbation of chronic pancreatitis.
An example of a menu for a week with pancreatitis
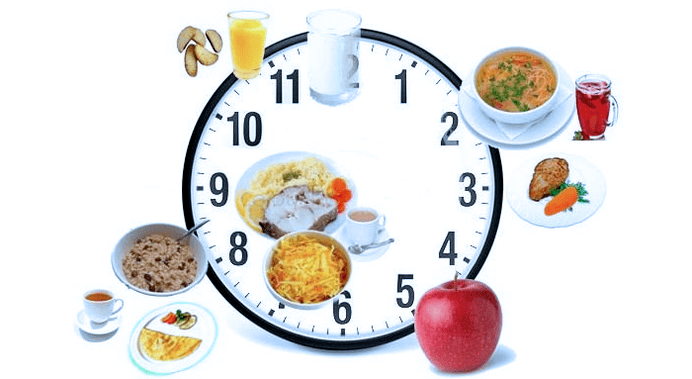
It is important to consider: no more than 200 grams of white bread and no more than 30 grams of sugar are allowed daily. You need to eat only fractionally, 6-8 times a day in small portions. It is advisable not to skip meals.
An example menu for pancreatitis for a week is given below.
Monday
- no more than 200 grams of mashed potatoes with 90-100 grams of meatballs, tea;
- no more than 100 grams of cottage cheese;
- carrot puree soup (no more than 250 grams), one toast, compote;
- 100 grams of steamed omelet (only from proteins! );
- a glass of yogurt.
Tuesday
- 150 grams of boiled fish and 150 grams of carrot puree, tea;
- no more than 100 grams of cottage cheese;
- 100 grams of steamed omelet;
- kefir.
Wednesday
- boiled fish with noodles (no more than 150 grams and only baked in the oven), 150 grams of puree;
- 100 grams of cottage cheese;
- soufflé from cottage cheese with tea (no more than 150 grams);
- a glass of yogurt.
Thursday
- 200 grams of mashed potatoes with the addition of steamed meatballs (no more than 10 grams), tea with milk;
- semolina milk soup (no more than 250 grams), fruit jelly;
- protein omelet (no more than 100 grams);
- curdled milk.
Friday
- apple and carrot pudding (no more than 200 grams);
- 250 grams of vegetable puree soup with compote;
- protein omelet (no more than 100 grams);
- curdled milk.
Saturday
- meatballs (no more than 100 grams) with mashed potatoes (no more than 150 grams), tea;
- protein omelet;
- grated oat soup (no more than 250 grams) with carrot puree (200 grams);
- curdled milk.
Sunday
- 160 grams of milk porridge from rice, tea;
- 200 grams of fruit jelly, 100 grams of boiled fish;
- curd pudding (no more than 150 grams) with rosehip decoction (150-200 grams);
- a glass of kefir.
Starvation
Fasting is very effective in acute pancreatitis or exacerbation of the chronic form of the disease. It is recommended to adhere to it in the described conditions for 1-3 days, using only ordinary water during this period.
Fasting is necessary to unload both the gastrointestinal system in general and the pancreas in particular. It is important to consider that during fasting, the use of broths, even low-fat ones, is not allowed.
















